-
drpvashistha@gmail.com
- +91 9004229819
Pancreatic Stent Placement in Mumbai, Navi Mumbai
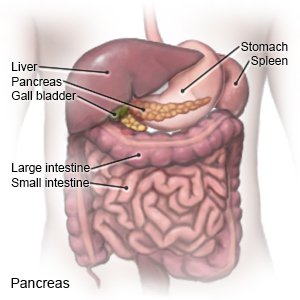
Pancreatic stent placement involves inserting a small tube, called a stent, into the pancreatic duct. This duct enables pancreatic juices to flow into the small intestine, aiding digestion. Stents are placed to relieve blockages or strictures in the duct, often caused by conditions like pancreatitis or cancer. The stent maintains the duct's openness, allowing normal pancreatic secretions to flow, reducing pain and preventing inflammation. This procedure is usually done during endoscopic retrograde cholangiopancreatography (ERCP), a minimally invasive technique combining endoscopy and X-ray imaging for diagnosing and treating digestive system issues.
Pancreatic Stent placement in Mumbai, Navi Mumbai is offered at Purushottam Vashistha Clinic. This procedure involves inserting a stent into the pancreatic duct to treat various pancreatic conditions. The clinic, under the expertise of Dr. Purushottam Vashistha, ensures advanced and compassionate care for patients requiring pancreatic interventions.
Located in both Mumbai and Navi Mumbai, the clinic provides convenient access to quality healthcare services. Trust Purushottam Vashistha Clinic for expert pancreatic care and stent placement in the bustling metropolitan region, promoting well-being and recovery.
Pancreatic Stent Surgery in Mumbai Navi Mumbai
Pancreatic stent placement is a medical treatment used to address pancreatic problems. During this procedure, a flexible tube-like structure called a stent is inserted into the pancreatic duct. The pancreatic duct is a passageway that carries digestive enzymes made by the pancreas to the small intestine.
Here are the key steps involved in pancreatic stent placement surgery:
-
Diagnosis and Evaluation:
- Before the procedure, the patient undergoes thorough diagnostic tests, such as imaging studies (CT scans, MRIs, or endoscopic ultrasound) to identify the pancreatic condition that requires treatment.
- The decision to place a pancreatic stent is typically based on conditions like pancreatic duct strictures, blockages, or leaks.
-
Preparation:
- The patient may be required to fast for a certain period before the surgery.
- Anesthesia is administered to ensure the patient is comfortable and pain-free during the procedure.
-
Access to the Pancreatic Duct:
- The surgeon may use different approaches for accessing the pancreatic duct, depending on the specific case.
- Endoscopic retrograde cholangiopancreatography (ERCP) is a common method. During ERCP, a flexible tube with a camera (endoscope) is passed through the mouth and into the small intestine, allowing the surgeon to visualize the pancreatic duct.
-
Stent Placement:
- Once the pancreatic duct is accessed, a contrast dye may be injected to enhance imaging.
- A guidewire is then passed through the stricture or blockage.
- Over the guidewire, the stent is inserted into the pancreatic duct to keep it open and facilitate the flow of pancreatic juices.
-
Verification:
- The surgeon confirms the correct placement of the stent using imaging techniques, ensuring it spans the affected area appropriately.
-
Postoperative Care:
- After the procedure, patients are monitored in a recovery area.
- Some patients may need to stay in the hospital for observation, while others can go home the same day.
Symptoms of Pancreatic Cancer
- Abdominal Pain: Pain or discomfort in the upper abdomen or back is a common symptom. This pain may become more pronounced as the cancer grows.
- Jaundice: Yellowing of the skin and eyes due to a buildup of bilirubin in the body. This can occur when the tumor blocks the bile ducts.
- Unexplained Weight Loss: Significant and unexplained weight loss can be a sign of various cancers, including pancreatic cancer.
- Loss of Appetite: A decreased interest in food and a loss of appetite can be associated with pancreatic cancer.
- Digestive Issues: Changes in bowel habits, such as light-colored stools, dark urine, or greasy and floating stools, may occur.
- New-Onset Diabetes: Diabetes that develops suddenly and without a clear cause may be associated with pancreatic cancer.